
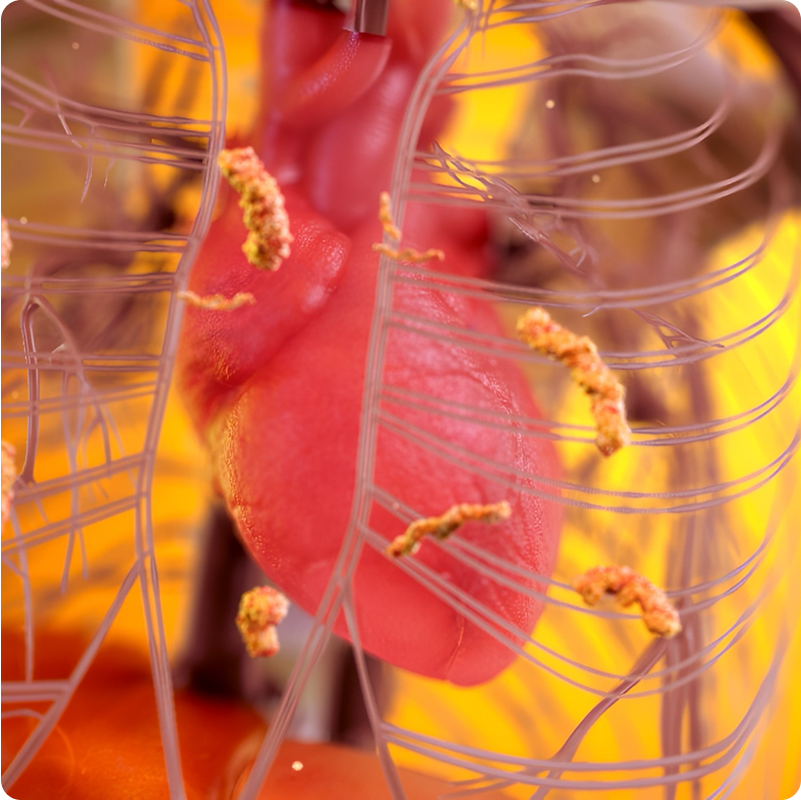
SUSPECTING ATTR
ATTR-CM is often overlooked as a cause of heart failure1-4
Prevalence of ATTR-CM in screening studies:
- In approximately 13-19% of people aged 60 or older with HFpEF, the underlying cause was ATTR-CM6-8
- Approximately 6 in 10 patients with ATTR-CM had bilateral carpal tunnel syndrome 5 to 10 years before cardiac manifestations9-12
- Approximately 1 in 6 patients with degenerative aortic stenosis was found to have ATTR deposition13,14
- Approximately 5-7% of patients with hypertrophic cardiomyopathy had ATTR‑CM15,16
*In a targeted literature review, mean time to diagnosis ranged from 1.3 to 7.2 years.
Men aged 60 years or older are particularly at risk of having ATTR-CM.13,17
Use echocardiography, electrocardiography, and cardiac MRIs to help raise clinical suspicion for patients with red-flag symptoms

- Left ventricular (LV) wall thickness ≥12 mm
- Thickening of valves/septum
- Refractile myocardium (granular sparkling)
- Presents in a "cherry-on-top" pattern
- Red indicates normal longitudinal strain at apex
- Pink and blue indicate abnormal longitudinal strain at mid/basal LV
- Abnormal E/A ratio, E/e' ratio, and TDI lateral e'
- 5-5-5 pattern in TDI tracings is seen in more advanced cardiac amyloidosis
- Presents in a "cherry-on-top" pattern
- Red indicates normal longitudinal strain at apex
- Pink and blue indicate abnormal longitudinal strain at mid/basal LV
- Abnormal E/A ratio, E/e' ratio, and TDI lateral e'
- 5-5-5 pattern in TDI tracings is seen in more advanced cardiac amyloidosis
- Low QRS voltage
- AV conduction block
- Pseudo-infarction
- Atrial arrhythmia
(eg, atrial fibrillation)
- Diffuse, subendocardial or transmural late gadolinium enhancement
- Left ventricular hypertrophy
- Increased extracellular volume fraction
References:
- Hanna M. Curr Heart Fail Rep. 2014;11(1):50-57.
- Mohty D, et al. Arch Cardiovasc Dis. 2013;106(10):528-540.
- Maurer MS, et al. Circ Heart Fail. 2019;12(9):e006075.
- Maurer MS, et al. J Am Coll Cardiol. 2016;68(2):161-172.
- Rozenbaum MH, et al. Cardiol Ther. 2021;10(1):141-159.
- Lo Presti S, et al. Crit Pathw Cardiol. 2019;18(4):195-199.
- González-López E, et al. Eur Heart J. 2015;36(38):2585-2594.
- Garcia-Pavia P, et al. Rev Esp Cardiol. 2025;78(4):301-310.
- Grogan M, et al. J Am Coll Cardiol. 2022;80(10):978-981.
- Milandri A, et al. Eur J Heart Fail. 2020;22(3):507-515.
- Ruberg FL, et al. J Am Coll Cardiol. 2019;73(22):2872-2891.
- Witteles RM, et al. JACC Heart Fail. 2019 Aug;7(8):709-716.
- Kittleson MM, et al. Circulation. 2020;142(1):e7-e22.
- Antonopoulos AS, et al. Euro J Heart Fail. 2022;24(9):1677-1696.
- Tomasoni D, et al. Front Cardiovasc Med. 2023;10.
- Aimo A, et al. Eur J Heart Fail. 2022;24(12):2342-2351.
- Nativi-Nicolau JN, et al. Heart Fail Rev. 2022;27(3):785-793.
- Dharmarajan K, et al. J Am Geriatr Soc. 2012;60(4):765-774.
- Dorbala S, et al. Circ Cardiovasc Imaging. 2021;14(7):e000029.
- Kittleson MM, et al. J Am Coll Cardiol. 2023;81(11):1076-1126.
- Maurer MS, et al. Circulation. 2017;135(14):1357-1377.
- Falk RH, et al. Heart Fail Rev. 2015;20(2):125-131.
- Baptista P, et al. Cureus. 2023;doi:10.7759/cureus.33364
- Cuddy S, et al. J Am Soc Echocardiogr. 2022;35(9):A31-A40.
- Maloberti A, et al. Int J Cardio Cardiovasc Risk Prev. 2024;21:200271.
- Quarta G, et al. Br J Radiol. 2011;84 Spec No 3(Spec Iss 3):S296-S305.
