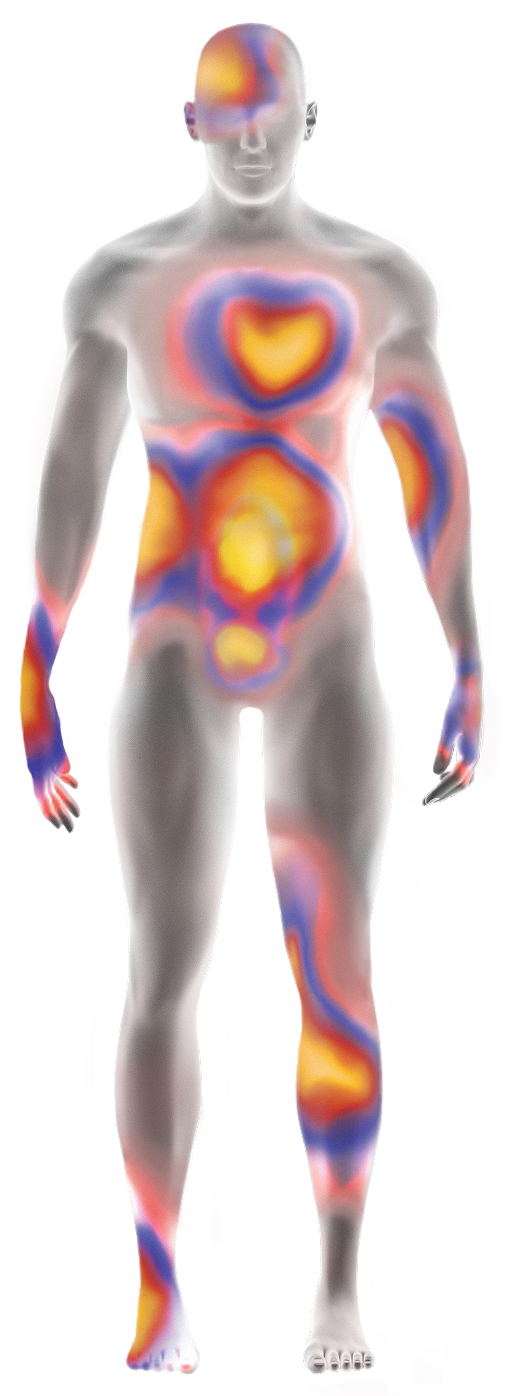
Multisystem involvement may be a sign of ATTR
ATTR develops primarily due to the accumulation of amyloid deposits in the heart and other tissues of the body. As the disease progresses, multisystem involvement may develop and should be considered a red flag.1-6
- Unexplained left ventricular (LV) wall thickening in the absence of hypertension
- Conduction system disease/atrial fibrillation
- Aortic stenosis
- HFpEF alone or in combination with other noncardiac red-flag symptoms
- Intolerance/suboptimal response to common cardiovascular medications, including HF treatments*
- Elevated NT-proBNP and troponin
- Shortness of breath
- Edema
- Altered sensation
- Difficulty walking
- Muscle weakness
- Numbness and tingling
- Autonomic nervous system disruptions (e.g., GI symptoms, orthostatic hypotension, recurrent UTIs, sexual dysfunction)
- Bilateral carpal tunnel syndrome
- Lumbar spinal stenosis
- Biceps tendon rupture
- Rotator cuff injury
- Trigger finger
- Vitreous opacification
- Glaucoma
- Abnormal conjunctival vessels
- Pupillary abnormalities
- Proteinuria
- Renal failure
*Patients with ATTR-CM can have intolerance to standard medications for heart failure, including ARNi, ACEi, ARB, or β blockers.
ACEi=angiotensin-converting enzyme inhibitor; ARB=angiotensin receptor blocker; ARNi=angiotensin receptor-neprilysin inhibitor; ATTR=transthyretin-mediated amyloidosis; ATTR-CM=cardiomyopathy of transthyretin-mediated amyloidosis; cMRI=cardiac magnetic resonance imaging; ECG=electrocardiography; echo=echocardiography; GI=gastrointestinal; HF=heart failure; HFpEF=heart failure with preserved ejection fraction; NT-proBNP=N-terminal prohormone of brain-type natriuretic peptide; UTI=urinary tract infection.
References:
- Koike H et al. Biomedicines. 2019;7(1):11.
- Adams D et al. Neurology. 2015;85(8):675-682.
- Adams D et al. Curr Opin Neurol. 2016;29(suppl 1):S14-S26.
- Mohty D et al. Arch Cardiovasc Dis. 2013;106(10):528-540.
- Garcia-Pavia P et al. Rev Esp Cardiol. 2025;78(4):301-310.
- Kittleson MM et al. J Am Coll Cardiol. 2023;81(11):1076-1126.
- Kittleson MM et al. Circulation. 2020;142(1):e7-e22.
- Maurer MS et al. Circ Heart Fail. 2019;12(9):e006075.
- González-López E et al. Eur Heart J. 2015;36(38):2585-2594.
- Maloberti A et al. Int J Cardiol Cardiovasc Risk Prev. 2024;21:200271.
- Dharmarajan K et al. J Am Geriatr Soc. 2012;60(4):765-774.
- Castaño A et al. Eur Heart J. 2017;38(38):2879-2887.
- Witteles RM et al. JACC Heart Fail. 2019 Aug;7(8):709-716.
- Conceição I et al. J Peripher Nerv Syst. 2016;21(1):5-9.
- Nativi-Nicolau JN et al. Heart Fail Rev. 2022;27(3):785-793.
- Brito D et al. Glob Heart. 2023;18(1):1-47.
- Mitter SS et al. ISA Congress 2020. Poster PT135.
- Maurer MS et al. J Am Coll Cardiol. 2016;68(2):161-172.
- Rozenbaum MH et al. Cardiol Ther. 2021;10(1):141-159.

